- MODULE 2: Working with ABI
- Introduction
- Take the Pre-test
- A. Uniquely building independence
- a) Unique
- b) Injury-Effect-Behaviour
- c) Frontal lobe proxy
- d) Change happens
in the day to day - e) A life span view
- f) Person centred, Goal directed
- B. Through emotions and relationships
- g) Person with ABI
- h) Family members
- i) Grief and loss
- j) Support workers
- k) Managers and Team leaders
- l) Case managers
- m) Professional boundaries
- C. With services
- n) Pathways
- o) Part of a team
- p) The services network
- D. Principles and standards
- q) Principles and standards
- E. Integration
- r) Practice tools
- s) Case study
- t) Further learning
- Take the Post-test
l) Case manager 
i) Case managers
Case managers also need to know a key to working with a person with an ABI is building a relationship with them. Working with people with acquired brain injury can be difficult.
Case managers also have to work with the person with the ABI and their family members in the grief process.
Case managers also have to change how they do case management to make it appropriate to working with people with ABI. They are also often involved in other services changing their work practices in order to provide a better service for people with ABI.
Changing one's own work practices and processes and practices of one's own and other organisations can be challenging.
Case managers need self-understanding about handling their own stress and what pushes their buttons.
Rules of thumb
1. Take time to get to know the person and their uniqueness.
2. Understand the connections between the injury, effect on their brain and effect on their behaviour.
3. You don't have to take behaviours personally.
4. Understand what pushes your buttons and develop strategies for dealing with this.
5. Understand your role with the person with ABI.
6. Understand how case management has to be different with people with ABI.
7. Identify your professional support network.
One case manager said:
What's the big thing that you have learned in the last six months in changing to case manager?
The biggest thing is to help maintain my stress levels and to be patient. To be more supportive to the other service coordination managers, the support workers and work as a team, because it is a big effort. You have got to rely on each other.
And the stress comes from?
Dealing with different clients with different issues. So it is that whole complexity around supporting a client, you get a whole lot of issues, especially when you have got more than one client who are having issues at any one time. So it is being able to manage your time, prioritise, and being able to de-brief with your team, it helps a lot too as well.
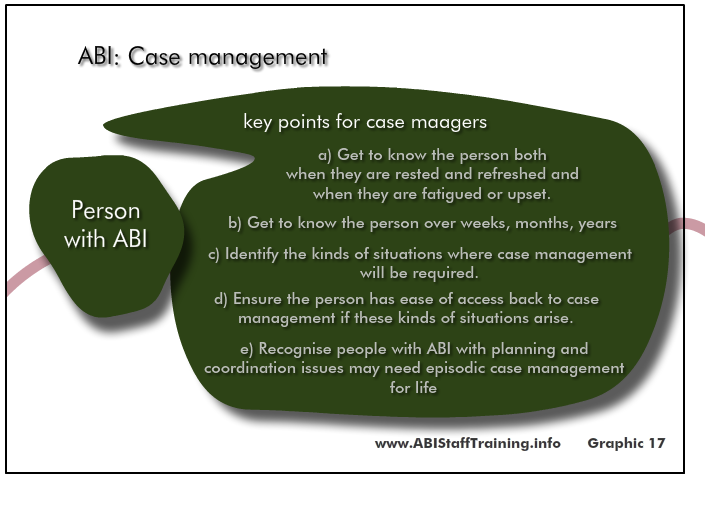
ii) Case management as needed
As noted above people who have damage to the frontal lobe of the brain often have difficulty with:
- planning
- coordinating
- initiating.
One of the consequences of this is that often people who have frontal lobe damage are also the ones who need ongoing case management. In these situations the Case manager's roles is to act as their frontal lobe.
One case manager noted:
When everything is running smoothing the person can seem to be functioning well. They may hold down a job, be able to get themselves to and from work. But if their job role were to change or if they had to decide whether or not to sell a property they are no longer able to cope. Case management is needed at this point.
Many people with an acquired brain injury and particularly those with frontal lobe damage will effectively require case management for life. In these situations case management is often not continuously required. It is required from time to time when planning, coordinating, decision making are required during periods of transition or change in circumstances (e.g. change of job, death of a carer).
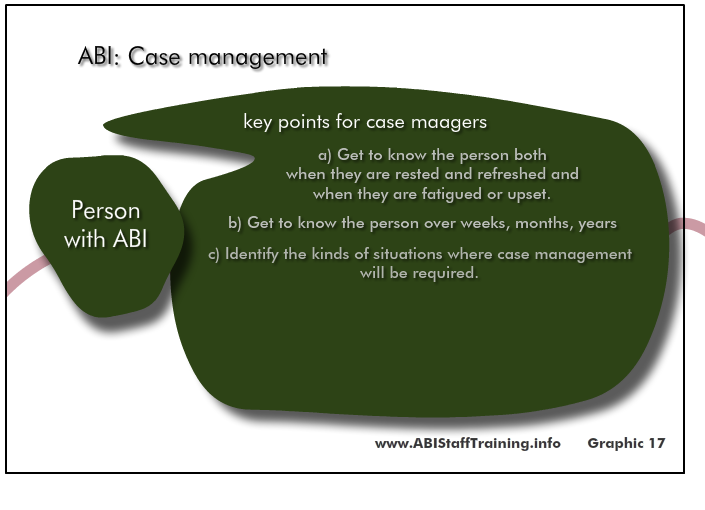
Rules of thumb
1. Get to know the person both over time and also for a period of time. Build trust and understanding. See how they are when they are fatigued and upset.
2. Identify the kinds of situations where case management will be required.
3. Ensure the person has ease of access back to case management if these kinds of situations arise.
A case manager said about her role as a case manager:
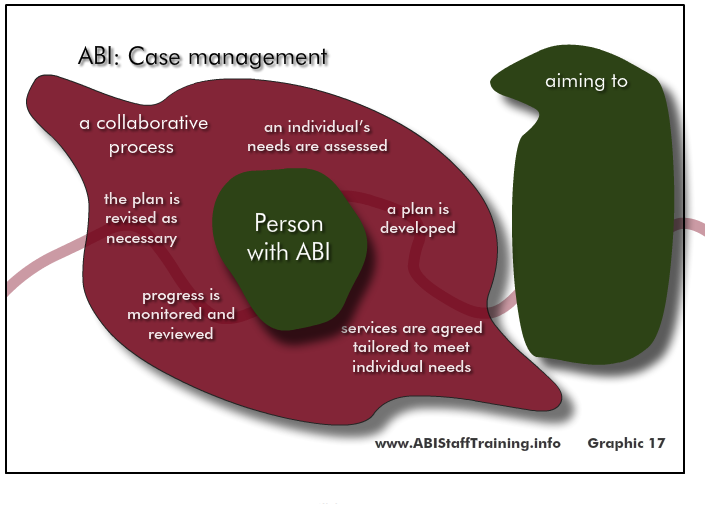
My role as a case manager entails managing a case load of clients with acquired brain injury and what that means is setting up individual programs for those clients.
So within that the central part of my role is to set up their individual service plans and for the clients, that means identifying their goals for the coming year. We do it on a yearly basis. And from that I can then plan their supports.
Beyond that my role also encompasses staffing. So I am involved in rostering, hiring and training new staff members, also in providing supervision. Within my role I also liaise with all the relevant bodies relating to a client. So that would mean medical practitioners, it would mean funding bodies, it would mean families, it would also mean any significant person to that client's life and coordinating services to them. So we set up appointments, we attend appointments and pass on relevant information as required.
We also are responsible for maintaining their budgets. We liaise with their funding body so we have to have an understanding of the financial aspects of their situations and then delivering services within those to meet their needs.
I spend some time out in the community supporting the clients and in that way I get a good grass roots understanding of the clients' needs and what it means to be a support worker out with those clients and how to direct new staff when they are first meeting that client.
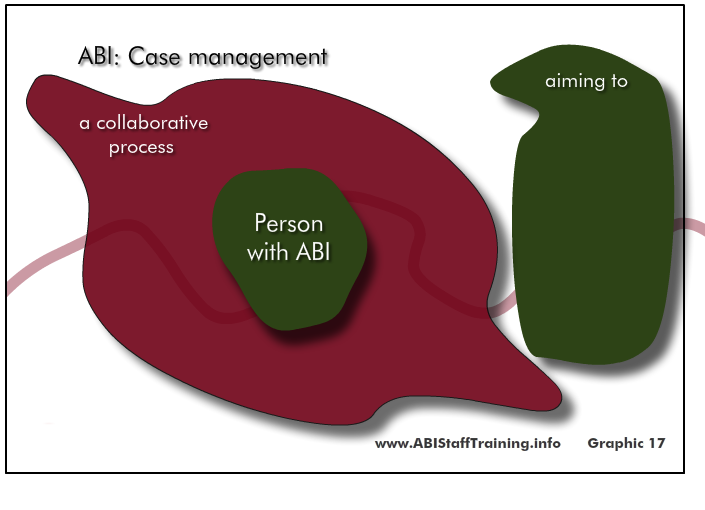
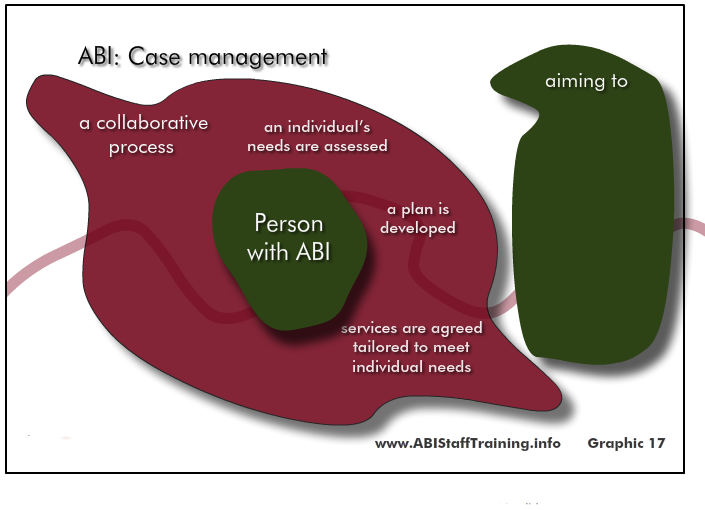
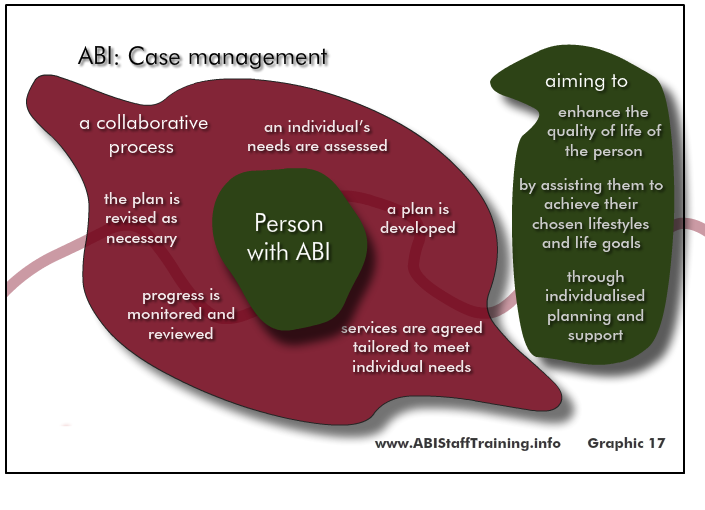
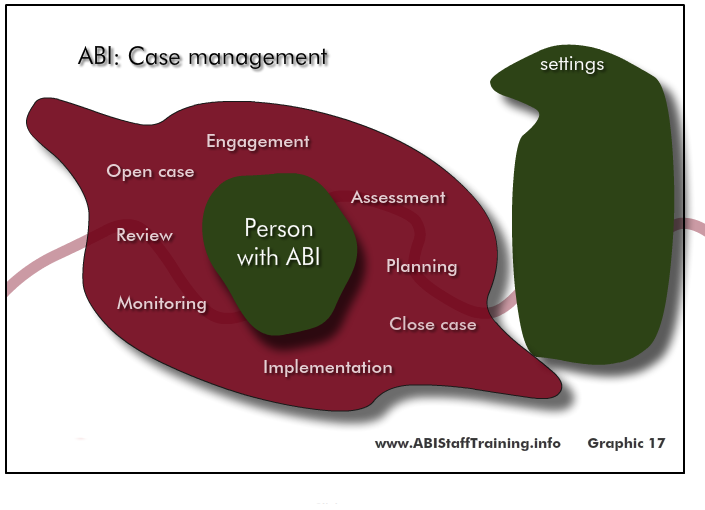
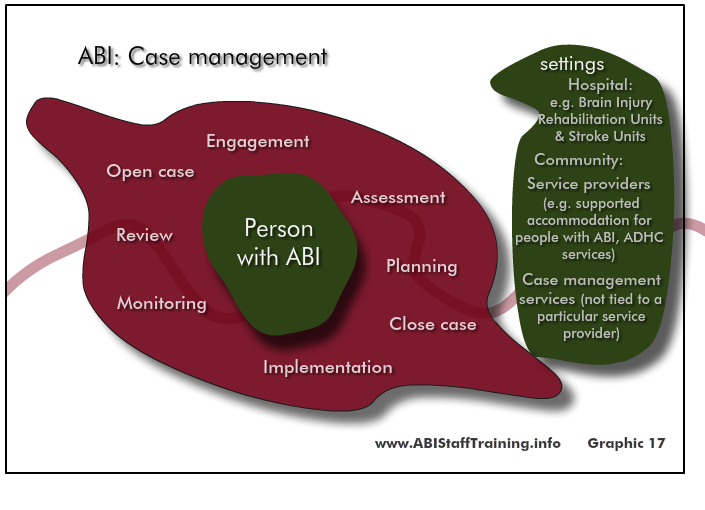
iii) Case management : Graphic
SLIDES:
To pause: Hover mouse over slide. To continue: move mouse off slide.
To go to a specific slide: Click on slide numbers below.
iv) Clip 17 : Case Manager : Experience Of Case Management (6 min)
A case manager talking about the experience of what it is like being a case manager.
v) Full text of the video Case managers' Story
ON SCREEN: Case Managers. JUDY.
JUDY: As a case manager my role is different every single day depending very much on the clients with whom I’m working at any given time and their needs.
ON SCREEN: JANE
JANE: My role as a case manager I see it as a project manager really. Putting together lots and lots of pieces.
ON SCREEN: LIZ
LIZ: The role of the case manager is really to synthesise and I guess coordinate all the services that the client is receiving in the community.
JANE: Obviously the client is the integral part of that, myself and the client. And that branches out to all of the rehab, and treatment, and care needs of that person are sort of we are at the top and all of that fits nicely hopefully around it whether it’s their occupational therapist, physio, GP, medical services specialists, neurology, operations, all of that sort of stuff and that also leads back into organisations like Life Time Care who are the funding body.
LIZ: So it’s kind of bringing together everyone and ensuring that all the services are coordinating to meet the goals I guess of the client in the community for their rehabilitation.
JUDY: I guess I see my job as making sure the safety net holds and supporting the client not only through that transition from hospital to home but then in setting up all the therapies that they may need when they go home, in organising the funding through Life Time Care for the services that they need be that care, or home modifications, or therapy, or anything really that is related to their injury.
JANE: So I really need to know what all of those bits are doing and work with a client on putting that together in a process for them that meets their rehabilitation goals.
JUDY: I say to clients when they ask “Mm, what exactly do you do?” I tell them “I’m the go-to-girl, if you are in doubt call me” because often that’s the way case management operates. We are problem solvers and hopefully in doing our job we take a lot of the stress and pressure off both the clients and their family.
ON SCREEN: As a Case Manager, Liz works alone…..
ON SCREEN: Jane and Judy work together as a two person small business
ON SCREEN: JUDY Case Manager
JUDY: When a client first goes home from hospital I would liken it to taking a new baby home. It is very anxiety provoking. They are leaving in freefall if you like with their injury for the first time. They may have had weekend leave prior to going home as a discharged person, but weekend leave doesn’t really prepare you I don’t think for that sense of being on your own. And no matter how good the case manager, no matter how supportive of the family I think that is a very scary time for both the client and their family.
ON SCREEN: LIZ Case Manager
LIZ: As the client was getting closer to discharge the rehabilitation team would identify a need for this person to receive attendant care services. And the rehabilitation team would assist the client or the family members in choosing an appropriate attendant care service that will assist their father, mother, daughter when they go home. That occurs as an inpatient because it’s important that the attendant care services does some training with the rehabilitation staff to understand what the needs are of the client that is about to be discharged home.
ON SCREEN: JANE Case Manager
JANE: It’s matching the attendant care worker with the skill that is required. So, with brain injury it may be more behavioural issues, with spinal cord injury it’s… well, the important stuff obviously is some health issues - their personal care, bowel regimes, how to lift people, OH&S issues, whether the house is modified. All of those sorts of things as well, which again can change. Someone may go home and their house may not be totally modified and equipment may still be arriving. So, it’s engaging the carers and working with the care agencies that the first few weeks, months or so may not be the ideal situation.
JUDY: With attendant care the client has hopefully spent some time meeting the carers and having dealings with them prior to going home. But essentially they are now receiving very personal assistance in very personal daily tasks from essentially strangers. And I think that's a huge adjustment for anyone. To have strangers coming into your home is confronting enough let alone to have those strangers seeing you naked and, you know, assisting you with dressing and toileting which are incredibly private things. And there is a sense because the carers are dressed in normal people’s cloths as opposed to a uniform that it’s different with nurses who are in an institution wearing a uniform. These are other people in your home wearing normal cloths and I think it’s really hard until a rapport develops between the client and the carer and they start to feel more comfortable and trust in each other. I think that first 6 weeks is really hard.
JANE: The first 6 weeks of someone being home with carers in the home is extremely difficult. And it’s shown that a lot of people, their families and the person may feel “We don’t need much care. Mum and dad are at home. I’ve got an older brother that pops in. We’ll be OK, and I’ll just have the minimal staff”. Again, I sort of keep a really open mind. It’s their choice. So, that’s what they’ve chosen when they are at hospital, even though they may get some counselling to suggest that that may not be realistic. But it’s still their choice. So, we let them go with that choice, but forever understanding that we could get a call at any time saying “Hey, this is really difficult, and we are not dealing with it”. That’s perfectly OK. Very acceptable as I said. Just because you go home with this today doesn’t mean that you can’t have something else the next week.
LIZ: Initially when people go home a lot of families and people living in the house find it very difficult to adjust to having a person that they don’t know in their house. It’s quite foreign to them. They also find it very difficult to understand exactly what their role is in regards to the care of the participant, of the client when they come home but also their role into providing the services such as, you know, making the evening meal that that person did pre-injury, that the goal of the attendant care worker would be also to assist in some meal preparation if that’s what the role of the client was before their injury.
JUDY: Clients also need to be aware that if for any reason they don’t feel comfortable with a carer, as long as it’s not that they just don’t like the colour of her hair or something, then they need to let the case manager know about that because no client should have to have a carer in their home that they are not comfortable with. And often in those early days, in that first little 6-week period there is a change in care staff for that reason.
ON SCREEN: Over time, as clients adjust to attendant care, usually it works well.
JUDY: Good morning. Judy
JUDY: As that trust in the carer develops and as the carer’s knowledge and instinctive feel for their client’s needs develops it almost becomes like a good marriage. You know, they are anticipation each other, they have got the trust in each other. And when care works well it can be fantastic. And it can really empower the client and the carer becomes like an unseen right hand, if you like.
ON SCREEN: Attendant carers do more than caring – they also help achieve rehab goals
JUDY: They have a modified vehicle, so that gets rid of that problem for you…
JUDY: So, over time what the care needs to do is work on being not just there to do for the client but to encourage the client and to facilitate them doing as much as they possibly can for themselves because care is a misnomer. Care should really be more about rehab than the care. Well, I mean it should be rehab with care. I’m not saying that. But it needs to be encouraging the client to do as much as they can for themselves and providing them with access to programs and exercises and equipment that the client may need to make that happen for themselves.
LIZ: They all developed a rehabilitation plan and that is very client focused and goal directed. The importance of the attendant care worker is to be able to assist in delivery of those goals. So, the goals are set in liaison with the client and the family. However, they may be an occupational therapy goal in regards to assistance and preparation of one evening meal a week. Part of the practice task could involve the attendant care worker being able to set the participant up, to be able to assist in some of the task to prepare their evening meal. So, the goal may be to be able to complete an evening meal one day a week in three months time. So, the attendant care worker will be given some task to be able to practice with a participant during the week to assist with the achievement of that goal.
JUDY: When I’m dealing with a client who has just gone home from hospital I will always arrange a team meeting and the carers are always a part of that meeting so that they are very across what the case manager and the therapists are trying to achieve and what the client wants to achieve as a result of their rehabilitation. Because the case manager is in and out of the client’s home, the therapists are in and out of the client’s home, the carer is the main stayer of the rehabilitation program really. And when care works well the carer is directing or implementing the goals that have been agreed by the client and the rehab team and providing the client with access to whatever they need to achieve those goals be it a daily exercise program, be it using the computer, be it hydro therapy, whatever.
ON SCREEN: Some common problems for attendant carers are boundary issues
LIZ: A lot of people struggle with what their role is and what the boundaries are. And ask the attendant care workers to do tasks that are outside their boundary such as making food for a family business, to sell in a family business or to be able to drive children to appointments when it wasn’t the role of the client pre-injury. And I think the family like the attendant care workers to become part of their family, to become friends. And that is very difficult for the attendant care worker when they are there that’s their work environment. And they are there as a professional to provide the attendant care services to the client in their home where the client and the family look at their environment as a home. So, it’s a work environment for the attendant care worker however it’s a home environment and a family environment for the participant and their family.
ON SCREEN: If things aren’t going well it is possible to change carers or care agency
JANE: Hello. Jane
JANE: During the whole course of someone’s care program there will be many changes of carers, hopefully not more than one at a time. In some instances though in saying that you may go from one agency to another agency. It may not be the carers that you are having a problem with. It may be something that the agency is not doing well that you just choose to go to another agency. Two different situations I guess if you choose a different agency. Some of those existing workers may transfer to that agency so you are taking a few of your core-workers with you. If it’s new carers within the same program the training of those carers again is integral. You know, you don’t just sort of meet someone and they start the next shift and just do buddy shifts with a carer. For them to even be introduced to you they should have at least the core TBI or spinal cord injury skills. So you know that they have had either experience or the agency is undergoing some current training with them.
ON SCREEN: These Case Managers find their jobs very fulfilling….
LIZ: I very much enjoy seeing the progress of the clients. A lot of these clients have been people that have lost all their independence and have in a very short period of time gone through a very tragic, catastrophic event.
ON SCREEN: And they look forward to no longer being needed by their clients.
LIZ: And to be able to see them gain their independence and start to interact and participate in community.
JUDY: I love my work. I love that every day is different. It brings different people. And I’m lucky. I’ve got really nice clients for the most part. Clients that I work well with. But I put a lot of work into developing that relationship too and trying to find out what the client wants and listening to what they want because sometimes when a client has a disability people stop listening. They talk to the client, they tell the client what they want, they tell the client what they should do whereas often the client has quite strong beliefs about what they want as well. And really that’s the important thing.
JANE: I do love it despite all of the pitfalls as well. Every day is different. Every client is different. And I think it’s the challenge and meeting those challenges which is my driving point. A lot of people say to me you know “How can you do this work?” They focus on the negativity, you know, “the poor person”. I see that in a sense sure that’s there but I focus on what I can help that person achieve. And it does happen.
JUDY: I see my job, and I say this to clients, as making myself redundant. If I have done my job well you will no longer need me because the structures have been put in place for you to live independently and for you to be able to manage your own rehabilitation. Because with the type of clients that I work with, the spinal cord injured and traumatic brain injured clients, rehab is going to be an ongoing life-long process. And they don’t want me in their life for all of that time. So, they may need me for a few years to set things up until they gain confidence in an understanding of what they need and how to achieve it. But after that I see I’ve done a good job if I can walk away and the client’s happy.
JANE: The Life Time Care are happy to provide him with that for the next 12 weeks with a real emphasis on him engaging in his rehab.
ON SCREEN: Thanks to Jane, Judy & Liz for taking part in this video. Camera & Editing Peter Kirkwood. Produced by Paul Bullen & Peter Kirkwood. www.living-with-attendant-care.info.
vi) Questions
Answer the following questions:
You are an experienced case manager. You are new to case managing ABI clients.
What are some of the emotional and relationship issues you will need to consider in relation to the client and their family and friends?
What are some of the emotional and relationship issues you will need to consider for yourself?
you will need to consider in relation to the client and their family and friends?
1.
A person with an acquired brain injury has had a life before the injury. Unless they are very young when they had the injury they will remember the life they had. They will have experienced loss and grief.
2. The acquired brain injury may have affected their
- thinking skills - cognitive
- communication/language
- physical/sensory
- emotional/behavioural/personality.
3. These can impact on their emotions - e.g. they may have a period of depression, they may have some personality change.
4. These emotional changes caused by the brain injury are not mental illness.
5. In addition to experiencing these changes the person with the ABI has to respond to and come to terms with their new life situation.
6. They also have to deal with their family members and friends coming to terms with the changes in them.
7. Friends often can't understand the changed nature of the person that they used to know and so friends fall away (even though their friendship is still very important to the person with the ABI).
you will need to consider for yourself?
1. It can be hard to get to know people with ABI - I need to give myself the time I need to do this.
2. Sometimes people with ABI can be abusive or aggressive or difficult to relate to in other ways. I need to not take this personally.
3. Gains with ABI clients can be slow in coming - I need to make sure I don't give up to soon. Or get caught in the disillusionment process.
4. Service providers are often not flexible enough for the needs of people with ABI. I will need to advocate on the behalf of people with ABI for services to be more flexible, change their policies to make them more appropriate. I may need to be ready for some fights.